Ahead of Hearing, Select Subcommittee Releases New Evidence of Dire Conditions at For-Profit Nursing Home Chains in 2020
Washington, D.C. (September 21, 2022) – Today, the Select Subcommittee on the Coronavirus Crisis, chaired by Rep. James E. Clyburn, released new evidence of dire conditions inside for‑profit nursing home chains during the early months of the pandemic, as well as documents that shed light on how convoluted corporate structures have been used by for-profit nursing home chains and may have helped these companies to obscure profits and avoid accountability. The new documents are being released in advance of today's scheduled 2 p.m. ET hearing entitled "Examining Long-Term Care in America: The Impact of the Coronavirus in Nursing Homes."
The Select Subcommittee has been investigating how large, for-profit nursing home chains have responded to the coronavirus pandemic. Today's release includes a selection of reports made directly to several major, for-profit nursing home chains from March through June 2020. These reports illustrate the horrors faced by nursing home residents and staff nationwide at the start of the pandemic.
New evidence released by the Select Subcommittee today includes the following key findings:
Many nursing home facilities were severely understaffed during the early months of the pandemic, leading to deficient care, neglect, and negative health outcomes for residents.
- Individuals at numerous facilities reported an insufficient number of nurses and certified nursing assistants (CNAs), resulting in staff members being responsible for dozens of nursing home residents at a time. For example, a SavaSeniorCare ("Sava") facility in Georgia had "one nurse to care for 35 residents per shift in the rehabilitation unit since the COVID-19 pandemic began" through at least June 9, 2020. A nurse at a Sava facility in Colorado reported that the facility had a ratio of "38 residents to one nurse" "every weekend" from October 2019 through March 26, 2020. According to the nurse, she raised concern about the staffing level to the facility's Director of Nursing but was told to "‘Deal with the issue because it is going to be like that for a while.'" One family member of a resident at another Sava facility in Georgia reported that there was "only one nurse and one CNA present for approximately 39 skilled nursing patients" as of April 14, 2020. The family member remarked that it was "‘criminal' for there to be so few staff members present."
- As a result of understaffing, numerous reports alleged that nursing home residents received deficient care and experienced neglect––leading to negative health outcomes. For example, one former resident reported that a Sava facility in Nevada had only one nurse covering two entire floors on April 7, 2020, and that a resident of this facility had vomited on herself and was not changed or showered until at least two days later, while another resident had to wait four hours for water. A report from the daughter of a resident at a Sava facility in California stated that there were "approximately 15 to 16 patients per nurse" as of June 9, 2020, and that her 95‑year-old mother had "experienced continuous delays receiving bathroom assistance and changing herself," which in part caused her to develop "an infection in her private area." According to the daughter, the resident had "not been provided satisfactory care because the facility is severely understaffed."
- While coronavirus outbreaks among staff may have contributed to staffing shortages in some facilities, one nursing home worker tied understaffing to corporate greed. An employee at a Sava facility in Colorado reported on March 25, 2020, that a manager "continues to under staff the building" and told employees that they were not permitted to increase the number of staff. The employee continued: "I understand the building needs to save money, but I feel we are being over worked and taken advantage of so administration can save money and look good to corporate."
For-profit nursing home chains did not supply their workers with adequate personal protective equipment (PPE)
- Staff and other stakeholders made numerous reports that employees and residents were provided with insufficient PPE during the early months of the pandemic––forcing them to utilize makeshift supplies to protect themselves. For example, at an Ensign Group ("Ensign") facility in Texas, an employee reported that staff were "told to share PPE with other employees" from April 13, 2020, through at least May 1, 2020. An anonymous individual reported that employees at a Sava facility in the Midwest had to wear the same masks for seven days in a row. Another report stated that, as late as May 8, 2020, employees at a Sava facility in Texas had to use "makeshift isolation gowns out of plastic paper [sic] bags" that were "stabled [sic] and taped together," while residents were "denied cloth mask[s] when asking for them" and instead were given "handkerchiefs" that did not properly fit and caused safety hazards when tied around some residents' necks. As late as June 26, 2020, an Ensign facility in California still had reportedly "failed to provide[] proper PPE/safety equipment or hand sanitizer despite having two positive COVID-19 cases."
Many nursing homes pressured staff to continue working despite having symptoms of or testing positive for the coronavirus—endangering nursing home residents and other staff.
- At many facilities, employees were reportedly pushed to continue to work while exhibiting coronavirus symptoms or testing positive. For example, a cook at a Sava facility in the Midwest was found to have a 101 degree fever during a temperature screening required to enter the building. The cook was reportedly instructed "to put a wet rag on her head before her temperature was taken again" in late April 2020. According to the report, lodged by another employee, the cook's "second temperature read 92 degrees and her first temperature was not recorded." The cook was then "allowed to work." At a Consulate Health Care ("Consulate") facility in Virginia, an employee who was initially sent home because of their "temperature level" was reportedly "instructed" by the Executive Director "to take Tylenol and come back to work." A staffing coordinator at an Ensign facility in Arizona was reportedly "making CNAs and nurses work despite reporting COVID symptoms, and refusing to let people call off when they report symptoms" as of June 26, 2020.
- Many reports highlighted a pattern of nursing home management threatening to fire or retaliate against employees if they called in sick. For example, in late April 2020, an employee of a Sava facility in Maryland reported that a colleague was "told . . . she would be terminated if she did not come to work," despite management's awareness that she had coronavirus symptoms. An individual reported that a manager at a Sava facility in Colorado was "pressuring employees . . . to work even if they feel bad and have concerns they may be sick with COVID-19," telling them "that ‘running a fever' was not a reason to call out of work" and urging them "not to share with their coworkers if they test positive for COVID-19."
- One employee reported that Sava's corporate offices ordered her termination after she had to stay home from work due to coronavirus symptoms and to take care of her children. The employee, who worked at a Sava facility in Georgia, reported that she had received approval to stay home to quarantine after experiencing coronavirus symptoms and to address her childcare needs by the facility's Director of Nursing, but later the Director of Nursing "said the corporate office told her she would have to terminate her [the employee]."
- Many facilities refused to give paid sick days to employees and contractors who needed to quarantine and did not require that employees quarantine despite testing positive, as then-existing CDC guidance recommended. For example, as late as May 22, 2020, management at a Sava facility in Colorado reportedly "informed the staff members they can continue to work even if they test positive for COVID-19." When an employee sought to stay home to quarantine, the facility's human resources department "refus[ed] to give her sick time" and instead required she use her paid time off to cover the time she spent in quarantine. Another Sava employee who had saved her paid time off because she needed to have a "major surgery" later that year reported that she was told by the payroll department that she would have to exhaust her regular paid time off after testing positive for the coronavirus before she could receive coronavirus-specific paid sick days.
For-profit nursing home chains' use of convoluted corporate structures may have helped to obscure profits and avoid legal and regulatory accountability.
- Internal company records from June 2020 reveal that for-profit nursing home companies included in the Select Subcommittee's investigation utilized convoluted corporate structures to own and operate their businesses. For example, Genesis Healthcare, Inc. ("Genesis")was comprised of over 700 discrete corporate entities as of June 2020, many of which acted as service providers to others within their family structure. According to Genesis' documents, many of these entities existed primarily to own interests in other Genesis entities, which in turn existed primarily to operate a discrete Genesis facility.
- These chains typically held each nursing home facility through one or more operating companies that were separated from the ultimate parent by many levels of corporate intermediaries. For example, as of June 2020, one Genesis facility was owned and operated by two separate corporate entities. While each of these two entities was ultimately owned by Genesis, there were eleven intermediate corporate entities separating them from their ultimate parent. The two entities that owned the facility did not fall under a common parent company until the fourth level of the corporate hierarchy.
- The figure below shows Genesis' organizational structure as of June 2020, and highlights the complexity and volume of entities making up a single nursing home chain.
Figure A: Corporate Organization of Genesis Healthcare, Inc. as of June 2020
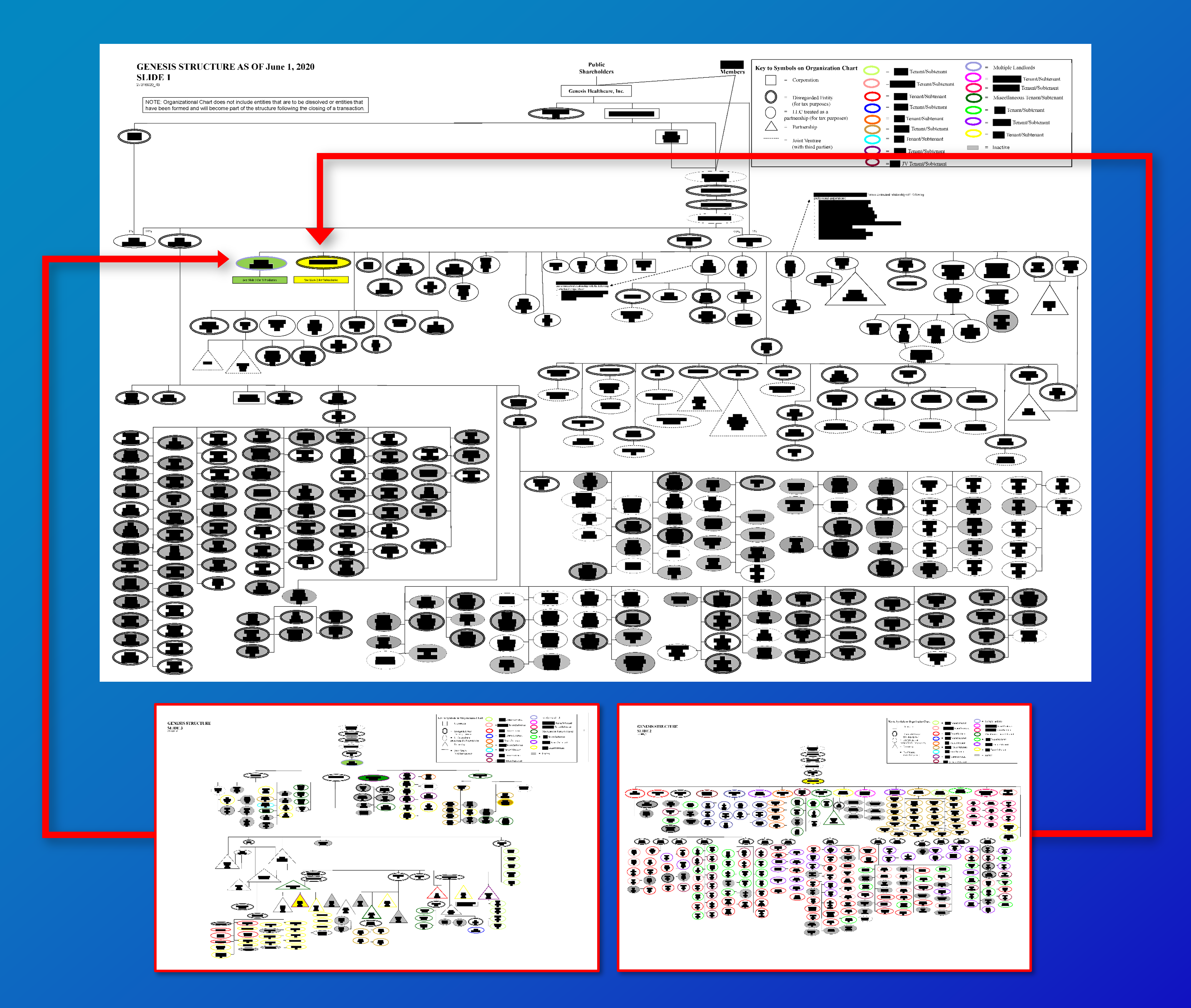
- The structure used by Genesis is consistent with those used by four other companies from which the Select Subcommittee obtained corporate documents. For example, Consulate described that it was structured as of June 2020, so that "Each facility is a stand-alone company that has its own employees, accounting systems, cost reports, etc." Consulate owns separate "Master Tenant" companies that hold facility leases and sublease facility premises to Consulate operating companies. Sava's corporate organization records similarly indicate that many or all of its facilities are held by discrete operating companies.
- Experts have indicated that because regulatory penalties and information regarding nursing home quality tend to be presented at the facility level—without an easily accessible way for the public to see ratings or infraction histories at the management or ownership level—convoluted corporate structures may serve to shield nursing home chains from close scrutiny by the public, including residents and their family members. Experts have also noted that the practice of nursing home parent companies using separate subsidiaries to service their operating companies may allow companies to obscure the true financial condition of a given nursing home facility. For-profit facilities have been found to deliver lower quality care and have been associated with worse health outcomes for residents.
- The corporate organization records received by the Select Subcommittee reflect the corporate organization structures for Genesis, Ensign, Consulate, Sava, and Life Care Centers of America ("Life Care") as of June 2020. Many of these companies have undergone significant reorganization since that time.
These documents were uncovered through the Select Subcommittee's ongoing investigation into five for-profit nursing home chains that collectively operated over 850 skilled nursing facilities charged with the care of over 80,000 residents as of June 2020, and each of which had significant coronavirus outbreaks across their facilities.
Click to read the documents released today: Selection of complaints from Ensign Group, SavaSeniorCare, and Consulate Health Care; corporate structure documents from Genesis HealthCare, Inc.; corporate structure documents from Ensign Group; corporate structure documents from Consulate Health Care; corporate structure documents from SavaSeniorCare; and corporate structure documents from Life Care Centers of America.